Eating Well With Diabetes: Practical, Medical, and Human-Centered Dietary Guidance
Diabetes changes your relationship with food—but it doesn’t have to break it. Too often, dietary advice for people with diabetes is framed as a long list of “don’ts,” leaving people feeling restricted, blamed, or disconnected from the joy of eating. That approach isn’t just emotionally exhausting—it’s medically unhelpful.
Food is not the enemy. Food is information. It communicates directly with your metabolism, your hormones, and your energy systems. When you understand how that conversation works, you gain tools—not rules—to support your health.
This article focuses on medical, evidence-based dietary recommendations for people living with diabetes, while honoring the reality that food is cultural, emotional, social, and deeply personal.
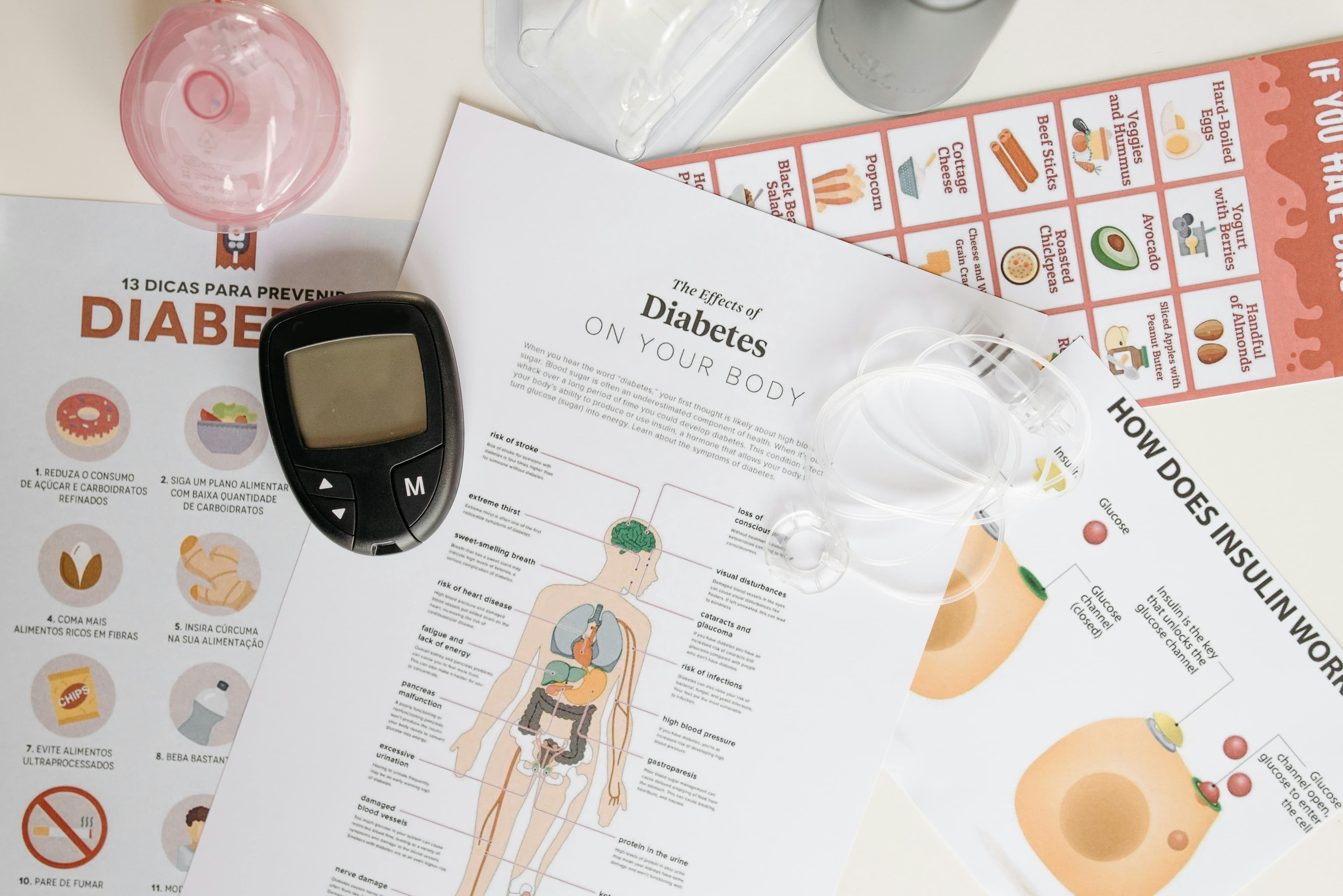
A Quick Medical Overview: Why Diet Matters in Diabetes
Diabetes—whether type 1, type 2, or other forms—affects how the body regulates blood glucose (sugar). Food, especially carbohydrates, has the most immediate impact on blood sugar levels.
Dietary choices influence:
- Post-meal blood glucose spikes
- Insulin needs or insulin sensitivity
- Energy levels and fatigue
- Weight stability
- Cardiovascular risk
- Long-term complications
The goal of dietary management is not perfection. It’s stability, predictability, and nourishment.
Carbohydrates: Not the Villain, But a Key Player
Carbohydrates raise blood glucose more than protein or fat, but eliminating them entirely is neither necessary nor recommended for most people.
Focus on carbohydrate quality
Medical guidelines consistently emphasize quality over quantity.
Better choices include:
- Whole grains (oats, brown rice, quinoa)
- Legumes (lentils, beans, chickpeas)
- Vegetables, especially non-starchy ones
- Whole fruits (in appropriate portions)
These foods contain fiber, which slows digestion and reduces blood sugar spikes.
Limit refined carbohydrates
Highly processed carbs tend to raise blood sugar quickly and sharply.
Examples to limit:
- Sugary drinks
- White bread and pastries
- Candy and sweets
- Highly processed snack foods
This doesn’t mean “never.” It means strategic and mindful use, ideally paired with protein or fat.
Fiber: One of the Most Underrated Tools
Fiber doesn’t raise blood sugar and helps regulate digestion, cholesterol, and satiety.
Medical recommendations often suggest:
- 25–38 grams of fiber per day, depending on age and sex
High-fiber diets are associated with:
- Better glucose control
- Improved gut health
- Reduced cardiovascular risk
Practical fiber sources:
- Vegetables
- Berries
- Nuts and seeds
- Whole grains
- Legumes
Increase fiber gradually and drink enough water to avoid digestive discomfort.
Protein: Stability and Satiety
Protein helps:
- Slow carbohydrate absorption
- Reduce post-meal blood sugar spikes
- Support muscle mass, especially important with aging or fitness training
Good protein options include:
- Fish and seafood
- Eggs
- Poultry
- Tofu and tempeh
- Greek yogurt
- Lean meats
- Legumes
Aim to include protein at every meal, not just dinner.
Fats: Choose Supportive Fats, Not Fear
Fat has minimal immediate impact on blood glucose, but it plays a major role in heart health—which is especially important for people with diabetes.
Prioritize unsaturated fats
Recommended options:
- Olive oil
- Avocados
- Nuts and seeds
- Fatty fish (salmon, sardines)
Limit saturated and trans fats
Excess intake increases cardiovascular risk.
Limit:
- Processed meats
- Fried foods
- Ultra-processed baked goods
Fat isn’t something to fear—it’s something to choose wisely.
Meal Timing and Consistency
Medical research shows that irregular eating patterns can worsen blood sugar control.
Helpful strategies include:
- Eating meals at consistent times
- Avoiding long fasting periods unless medically supervised
- Balancing meals with carbs, protein, and fat
For people using insulin or certain medications, consistent timing helps reduce the risk of hypoglycemia (low blood sugar).
Portion Awareness Without Obsession
Portion size matters—but obsession doesn’t help.
Medical nutrition therapy focuses on:
- Plate-based approaches (half vegetables, one-quarter protein, one-quarter carbohydrates)
- Visual cues rather than constant counting
- Flexibility over rigidity
This supports long-term adherence and mental well-being.
Sweeteners and Sugar Alternatives
Non-nutritive sweeteners can help reduce sugar intake, but moderation matters.
Medical guidance suggests:
- Use sweeteners as tools, not replacements for balanced eating
- Monitor individual blood glucose responses
Everyone reacts differently—personal data matters more than blanket rules.
Special Considerations for Physical Activity
For people who train or exercise regularly:
- Carbohydrates may be needed to prevent low blood sugar
- Pre- and post-workout nutrition should be individualized
- Hydration is critical
Exercise improves insulin sensitivity, but nutrition must support it safely.
Cultural and Emotional Realities of Food
Food is memory, tradition, and connection. Medical recommendations that ignore culture often fail.
Sustainable diabetes care:
- Adapts traditional foods rather than eliminating them
- Focuses on preparation methods and portion balance
- Respects emotional relationships with food
There is no single “diabetes diet.” There is your diet, supported medically.
When to Seek Professional Guidance
Dietary needs vary based on:
- Type of diabetes
- Medications or insulin use
- Pregnancy
- Kidney or heart conditions
- Eating disorder history
A registered dietitian or diabetes educator can personalize recommendations safely and effectively.
A Compassionate Closing Thought
Managing diabetes through diet is not about control—it’s about collaboration between you, your body, and your medical care.
You don’t need perfect meals.
You don’t need food guilt.
You don’t need to earn your health.
You need nourishment, information, consistency, and compassion—for yourself.
Food can still be pleasure.
Food can still be culture.
Food can still be freedom.
With the right knowledge and support, eating with diabetes becomes not a restriction—but a powerful form of care.
About the Author
Studio Citylines Health Desk
Certified Fitness Professional & Nutrition Specialist
Expert fitness professional with over 10 years of experience helping people achieve their health and fitness goals through evidence-based training and nutrition. Certified by ACSM and NASM with specializations in weight management and sports performance.